Vaccination in the Era of Covid
Perspectives and Practices of Health Care Workers; Award-Winning Research Points to Need for Education at All Levels
Atif Towheed remembers it well—the end of the fall semester one year ago at Touro College of Osteopathic Medicine (TouroCOM) in Middletown. Saying good-bye to a classmate in their second-year Clinical Systems course, he asked her, “Have you gotten your annual flu shot yet?”
“No, I don’t get flu shots. I never get the flu,” he recalls the student saying. “I also think I might get sick with the flu if I get a flu shot.”
The reply took him by surprise, coming from an aspiring physician. “She didn’t give any of the recognized excuses, like religious beliefs or a standard medical exemption. I was shocked,” he recalls.
Beginning of a Journey
The incident marked the beginning for Towheed, now a third-year medical student, of what would soon become a journey to learn more about health care providers’ attitudes towards vaccinations. Working with a team from TouroCOM and the local health department, he would take the lead in award-winning research that continues to this day, as news reports proliferate about physicians and nurses rejecting the COVID-19 vaccine.
In New York, Governor Andrew Cuomo reported that about 15 percent of nursing home staff declined the COVID-19 vaccine, as administration entered its third week. According to the Los Angeles Times, a survey by Kaiser Family Foundation in December found 29 percent of health care workers were “vaccine hesitant,” a figure slightly higher than the 27 percent reported in the general population.
Among the top reasons given for the skepticism were safety concerns. “A lot of people, including health care providers, feel that the development of the vaccines was a little bit rushed,” says Towheed. “At least two nurses with whom I worked directly, on separate occasions, rejected the COVID-19 vaccine. One of the major hurdles is an inability to distinguish facts versus misinformation.”
Measles Outbreak Sparks Collaboration
In 2019, New York State was hit by one of the largest measles outbreaks since the 1990s. Highly publicized anti-vaccine campaigns were waged throughout the state and the nation. Towheed, with fourth-year DO student Anna Tran, faculty advisors Dr. Stephanie Zeszutek and Dr. Adetokunbo Shobaloju, and Lissette McNulty, a nurse from the local health department, decided to research health care workers’ attitudes and practices related to vaccination.
Research, including on coronaviruses, is not new to Towheed. After receiving his master’s degree in biotechnology in his native India, he joined a United Nations research lab where he studied viruses, including the now-infamous SARS coronavirus. In 2009, he came to the United States, where he earned a Ph.D. at the University of Pittsburgh School of Medicine and completed a postdoctoral fellowship at the Children’s Hospital of Philadelphia. During this time, he studied and evaluated gene therapy for mitochondrial diseases, including a potential treatment for vision loss due to genetic mutations.
The opportunity to investigate vaccine compliance while the world was on the precipice of new vaccine discoveries for COVID-19 proved irresistible. “Our team discussed among ourselves how increasing compliance could lower health care costs, especially given the increasing number of vaccine-preventable diseases in the United States,” he explained.
Award-Winning Survey Launched
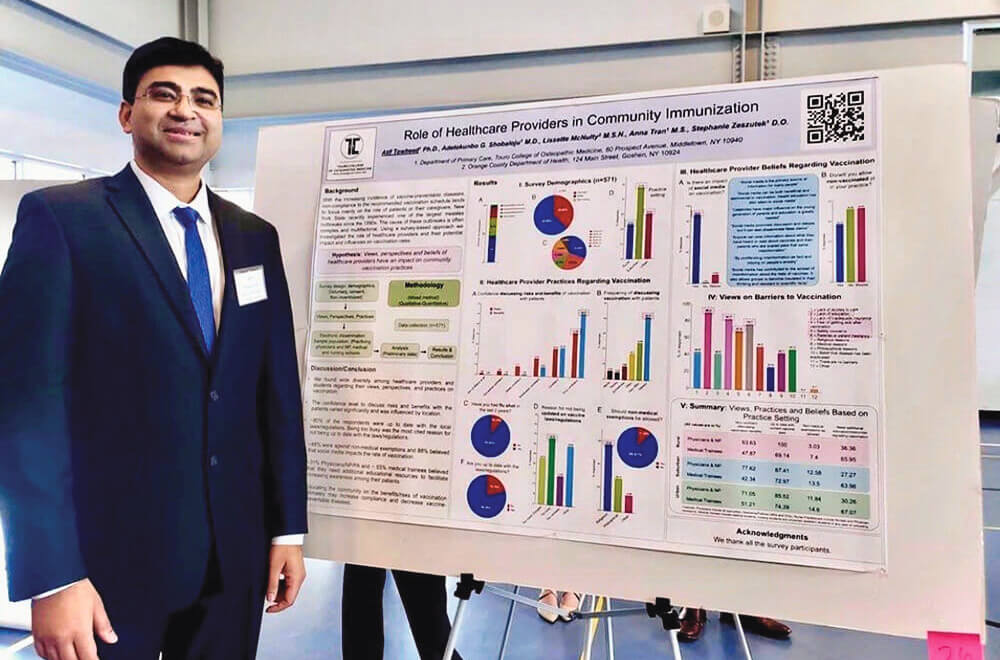
Beginning in Summer 2019 and through the fall, the team surveyed a diverse population of health care workers and students about their practices and beliefs related to vaccination, and how these might impact vaccine compliance. Their work, first published as a poster entitled “The Role of Health Care Providers in Community Immunization”, impressed the American Osteopathic Foundation (AOF) and garnered recognition for Towheed in the form of an AOF Student Researcher Award last November.
Their survey focused on health care practitioners and trainees throughout the U.S. Forty-five percent of the 571 respondents were medical students, 32 percent were physicians, and 15 percent were nursing and allied health professionals. Respondents lived and worked in rural, suburban and urban settings.
Among other things, they explored how often practitioners talk about vaccination with patients and their confidence levels in doing so. Also examined were providers’ views and beliefs as they relate to immunization.
Among the Highlights:
- 41% of respondents reported always discussing vaccines with their patients
- 30% were either unsure about vaccines or would not recommend them
- 36% said they would not allow unvaccinated patients in their practice, while 28% said they would treat such patients
- 88% opposed non-medical exemptions for vaccines
- 88% believed social media impacts vaccination
- Half of the respondents reported a need for more education about vaccines, both for themselves and patients
The top barriers to vaccination identified by respondents were lack of education, fear of becoming sick, parental or patient hesitancy and safety concerns. Lack of confidence in discussing vaccines is likely a barrier as well, Towheed said. Eighty-seven percent of respondents said they were “confident to very confident” discussing the benefits of vaccines, yet only 68 percent expressed that same level of confidence discussing the risks.
Targeted Education Needed for All
Among the team’s recommendations were increasing awareness about vaccination through education programs targeted at health professionals at different levels of their education and careers. Towheed also believes more research is needed on the impact of social media on immunization.
With more education, they assert, vaccination rates will improve, and the numbers of preventable diseases will decline, saving lives and reducing health care costs. “Having discussions, expressing concerns and having those concerns addressed by people knowledgeable in the field is what’s needed,” Towheed concludes, adding he also plans to continue his journey exploring the practices of health care providers. “I am launching a new project studying the reasons for their low COVID-19 vaccine rates.”

